Tiffany M. Chapman, B.S., Idania B. Brown, B.A., Angel Arizpe, B.S., Claudia M. Toledo-Corral, Ph.D., Department of Health Sciences, California State University, Northridge, Northridge, CA
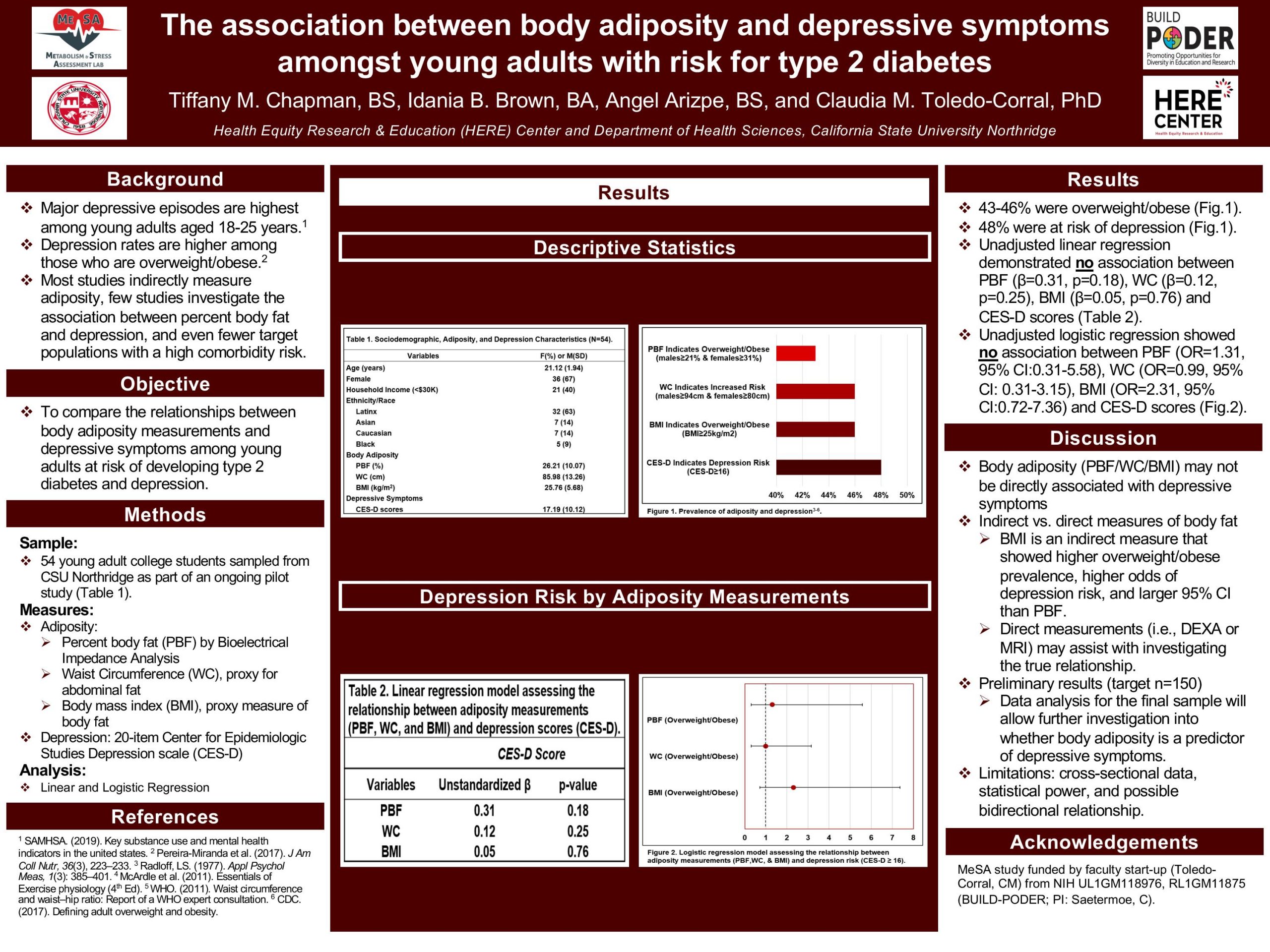
Background: Depression is one of the most common mental health conditions in the United States and major depressive episodes are highest among young adults aged 18-25 years. Depression also co-occurs with other physical health conditions, such as obesity which has been on a steady rise. Few studies investigate the association between percent body fat (PBF) and depression and even fewer target populations with high comorbidity risk. The study objective is to compare the relationships between body adiposity measurements and depressive symptoms among young adults at risk of developing type 2 diabetes and depression.
Methods: The Metabolism and Stress Assessment (MeSA) lab is currently recruiting California State University, Northridge students ages 18-25 years old with a family history of type 2 diabetes. Obesity is being evaluated using body mass index (BMI) and PBF measured by bioelectrical impedance analysis. Depressive symptoms are being evaluated using the 20-item Center for Epidemiologic Studies Depression (CES-D) Scale with a score of 16 or greater indicating depression risk. Point-Biserial correlation assessed the relationship between BMI (kg/m2), PBF, and CES-D scores.
Results: The preliminary sample (n=24) was comprised of 66.7% female, 56.5% Hispanic or Latino/a, 21.7% Asian, 13.0% Caucasian, and 8.7% Black. 45.8% of the sample were at risk for depression and 62.5% were overweight/obese. The sample had a mean of 21.33 years (SD=1.83), 26.56 kg/m2 (SD=5.86), 26.79 PBF (SD=9.28), and 16.29 CES-D score (SD=8.90). Preliminary results found that BMI was marginally associated with depression risk (r=0.40,p=0.05), while PBF was not (r=-0.01,p=0.96).
Conclusion: The results of this ongoing study showed that BMI may be associated with depressive symptoms. Data analysis for the final sample (n=100) will increase statistical power and decrease possibility of type II errors. This will allow us to further investigate whether body adiposity is a predictor of depression and provide promising implications for prevention strategies among this at-risk population.
*This poster was presented at The American Psychosomatic Society annual meeting. The sample size reflects that of March 2020.